covid
Long COVID’s Impact On The Brain

Deciphering your sniffles and sneezes through a pandemic.
5 min read
Life in the time of COVID-19 has many of us overanalyzing every throat tickle, sneeze, and, sometimes, even our stool. Should I be concerned about that nose drip? Is my chest tightness anxiety? Or a symptom of something else?
With the unknowns of the pandemic plaguing us all, some people are worried that even mild symptoms are a sign of the virus. Having allergy season in full swing only adds more confusion to the mix, making it even harder to tell the difference between COVID and seasonal allergies. And while colds and flus may be miserable but mostly harmless, you fret that they share common symptoms as the novel coronavirus.
Fortunately, amid the similarities of colds, flus, allergies, and coronavirus, there are some key differences.
Luckily, the main signs of allergies—itchy, watery eyes, along with sneezing, postnasal drip, nasal congestion, and running nose—are atypical indicators for COVID.
Another key clue: You have a history of previous spring or fall time allergies. However, “There are many patients who present with new-onset allergy symptoms each year, which may lead to some confusion and anxiety,” says Mitchell Boxer, MD, an allergy and immunologist with Northwell Health, and assistant professor at the Zucker School of Medicine at Hofstra/Northwell.
Discuss your symptoms with your primary care provider (PCP) or allergist to determine an appropriate treatment plan, Boxer advises. There are many effective over-the-counter or prescribed medications that can help reduce allergy symptoms.
“With the general public on edge, this is not a good time for anyone to be coughing and/or sneezing in a public environment,” Boxer says. While people with allergies are at no greater risk of getting COVID, if they do have it and are coughing and sneezing in public, this is potentially problematic. That’s because wearing a mask does not completely prevent aerosolized particles from escaping through the openings of the mask.
A run-of-the-mill cold can also present with postnasal drip, runny nose, sneezing, sore throat, nasal congestion, watery eyes, and low-grade fever. An important difference is the lack of itching of the eyes and nose, Boxer says. Normal colds last anywhere from two to four days. If you find your illness lasting longer and the symptoms more severe than a routine cold, it is possible you may have the coronavirus.
Depending on the severity of a person’s case, the average flu can present with symptoms such as fever, headaches, body aches, sore throat, runny nose, stuffed sinuses, coughing, sneezing, and occasionally vomiting and diarrhea. While many symptoms of COVID and the flu overlap, an important difference between the two is the sudden loss of smell in many COVID patients, Boxer says. If someone believes they are experiencing flu-like symptoms, the sooner you can get tested, the better, he explains. That’s because there are tests—such as a respiratory viral panel—that can test for influenza A and B, RSV, and COVID, as well as antiviral medications that “can be used to shorten and potentially lessen the severity of influenza.”
And while COVID-era precautions such as mask wearing, social distancing, and washing hands will help to also reduce the spread of influenza, Boxer says it is particularly important for patients to get the flu vaccine this year. This, he explains, is especially critical as the two are “separate distinct viruses, and therefore it is possible for a patient to get both COVID and influenza.”
If you are experiencing flu-like symptoms with worsening shortness of breath and chest pain, Boxer advises seeking emergency medical care.
The most common symptoms of COVID include fever, cough, shortness of breath, fatigue, loss of appetite, chills, body aches, headache, sore throat, and loss of taste or smell, Boxer says. Less commonly, people may experience a runny nose, nausea, vomiting or diarrhea, dizziness, confusion, seizures, stroke, tingling or numbness in the hands or feet, and rashes.
Symptoms can vary depending upon the age of the individual and will develop within two to 14 days after exposure to COVID.
If you suspect you have COVID, the first step is to contact your physician for further advice, Boxer advises. Most people with COVID can manage their illness and recover at home without medical care.
“Your doctor should have a protocol in place to keep track of your symptoms through the course of the illness and will advise you accordingly about what symptoms need to be addressed urgently,” Boxer says.
Staying hydrated is crucial; Boxer recommends stocking up on either Gatorade or other supplemental fluids. “It is also important to get out of bed regularly despite not being motivated to do so,” he says. Your physician will advise you on breathing exercises that should be done regularly to attempt to lessen COVID effects on the airways.
In New York, if you have a fever, cough, chills, and body aches, you are presumed to have COVID and should be treated as such. Patients are advised to contact their doctor to discuss and will most likely be referred to a local testing center for further advice. Information about being tested at a Northwell Health center is available by calling (833) 487-2273.
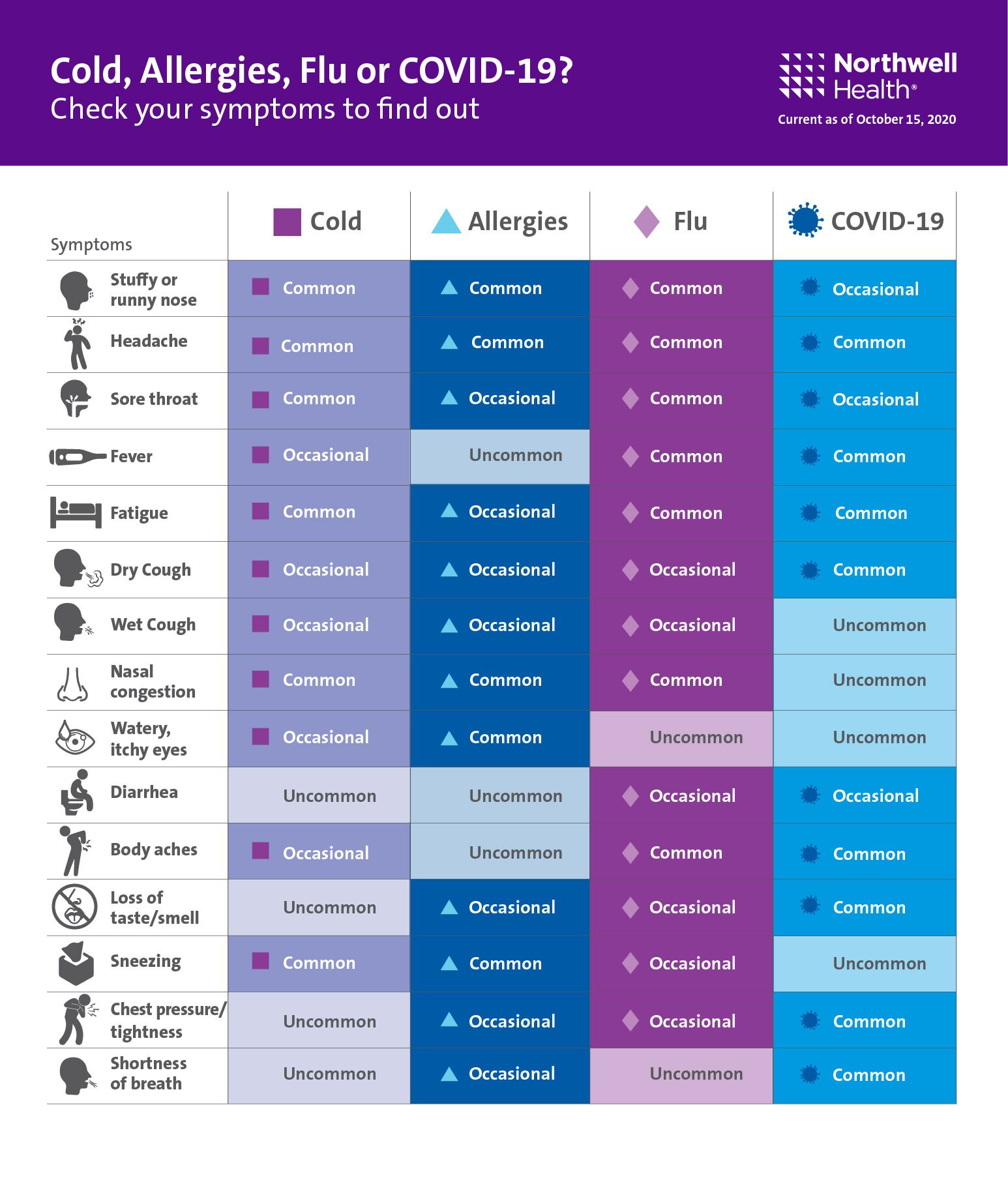
You may find the chart below useful to help you decide if you are wondering if your symptoms require further medical care:
Subscribe here to receive alerts for all things coronavirus and more from The Well.
The Well is Northwell Health’s commitment to the future of health care. In this time of information overabundance, much of which is inaccurate, unhelpful, or even difficult to understand, Northwell Health is on a mission to make a difference as an honest, trusted, and caring partner. The site connects with consumers to provide them with personalized content that reduces their stress, makes them laugh, and ultimately feel more confident and capable on their healthcare journey.